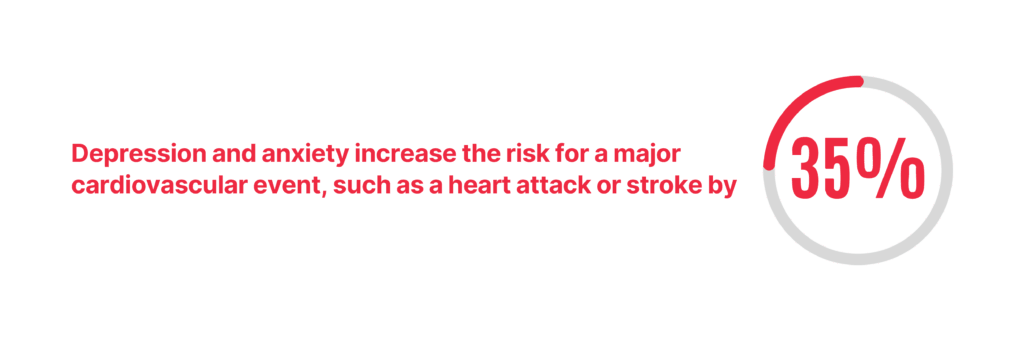
All human beings eventually learn that life’s challenges—whether the loss of a loved one, job instability, or the end of a meaningful relationship—take an undeniable toll on mental well-being. But the effects don’t stop there. Research shows a strong connection between psychological distress and physical health, particularly cardiovascular disease. A 2024 study out of Boston’s Massachusetts General Hospital, for example, found that depression and anxiety increase the risk for a major cardiovascular event, such as a heart attack or stroke, by about 35%. A 2023 study by researchers at Johns Hopkins University likewise concluded that people who self-report feeling depressed or having poor mental health days have higher rates of heart attacks, strokes, and risk factors for heart disease compared to their peers who lack mental health issues.
The same mind-body connection that researchers have discovered in the heart can manifest in myriad ways across the entire anatomy, according to board-certified emergency medicine physician John Lucas, DO, founding dean and chief academic officer of the Illinois College of Osteopathic Medicine (IllinoisCOM) at The Chicago School. When it welcomes its first class of students, IllinoisCOM will therefore make mental health a major focus of its culture and curriculum, Dr. Lucas says. Not in spite of being a medical school, but because of it.
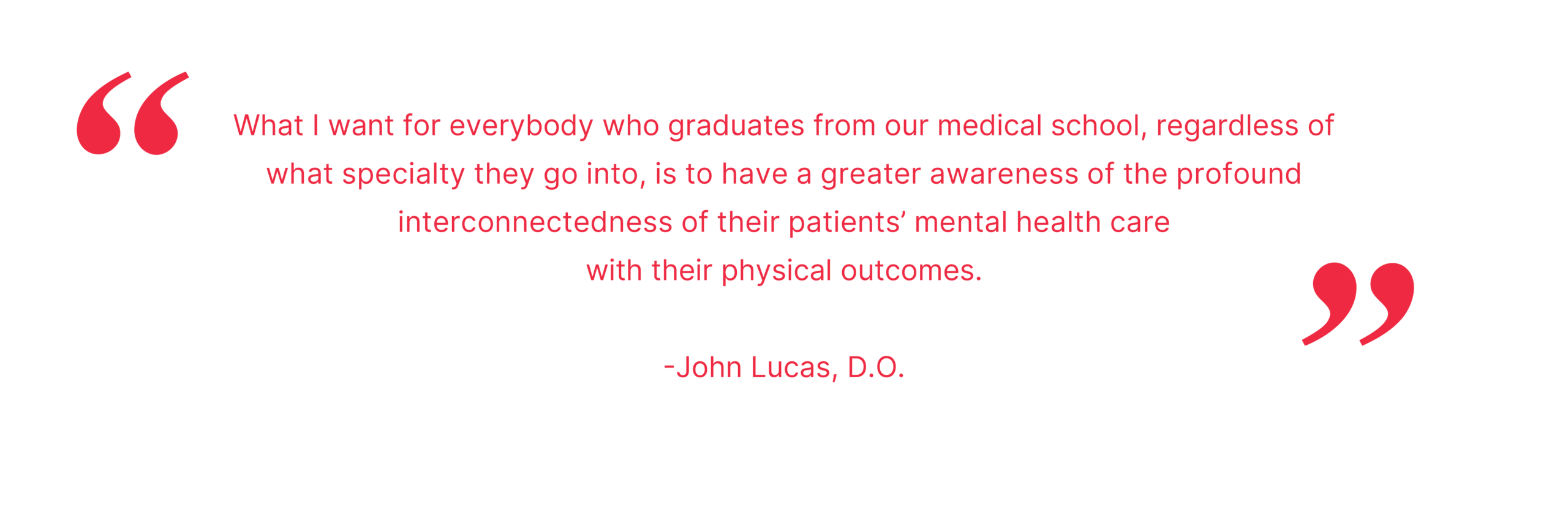
“More than 50% of people who seek mental health care for the first time do so with their primary care doctor, yet a lot of primary care doctors have inadequate preparation in the behavioral healthcare arena,” Dr. Lucas observes. A 2021 study published in the Journal of Primary Care & Community Health states that, in fact, the percentage of patients seeking mental health care who receive it from their PCP is close to 60%. “What I want for everybody who graduates from our medical school, regardless of what specialty they go into, is to have a greater awareness of the profound interconnectedness of their patients’ mental health care with their physical outcomes.”
To improve outcomes not only for patients who need mental health care, but also for the communities in which they reside—where a lack of mental health care can manifest in the form of public health concerns like unemployment, poverty, substance abuse, homelessness, family dysfunction, and crime, just to name a few—the nation desperately needs to deepen its bench of mental health care providers, echoes Monica Kinde, Ph.D., senior associate dean of preclinical affairs at the IllinoisCOM.
“Patients these days have to be very self-directed when it comes to seeking healthcare, including mental health care. And very frequently, the primary person—and sometimes the only person—a patient will touch is their primary care provider,” Dr. Kinde says. “For that reason, it’s really important that we train more primary care providers who are ready and willing to talk about mental health, to intercept patients who have mental and behavioral health challenges, and to effectively refer those patients to the appropriate providers and manage treatment in the primary care setting when necessary.”
A Country in Crisis
Mental health care is more important today than it’s ever been. Just consider the following facts:
- Nearly a quarter of adults (23%), or nearly 60 million Americans, live with mental illness, according to Mental Health America (MHA), a nonprofit whose mission is advocating for mental health and well-being. Less than half (47.2%) have received treatment, adds the National Alliance on Mental Illness (NAMI).
- A third of those with mental illness also struggle with a substance use disorder, according to NAMI. Nearly two in 10 American adults (18%) had a substance use disorder in the past year, and the majority (77%) did not receive treatment, MHA adds.
- More than 5% of the U.S. adult population, or approximately 12.8 million people, say they’ve experienced serious thoughts of suicide, MHA reports. And in 2022—the most recent year for which there is data—a record 49,500 Americans died by suicide, reports the U.S. Centers for Disease Control and Prevention (CDC).
- One in five (21.1%) people experiencing homelessness in the United States has a serious mental health condition, NAMI says.
- Serious mental illness costs the U.S. economy $193.2 billion in lost earnings each year, according to NAMI, which says depression and anxiety disorders likewise cost the global economy $1 trillion in lost productivity each year.
A Holistic and Preventative Approach
The emphasis that osteopathic medicine puts on holistic and preventative care will make the IllinoisCOM an ideal vehicle through which to train physicians who are fluent enough in mental health care to serve on the front lines of the nation’s mental health crisis.
“We’re not just developing a medical school. Specifically, we’re developing an osteopathic medical school,” Dr. Lucas explains. “Osteopathic physicians embody all the traditional teachings of medicine and are licensed and credentialed to practice all the different specialties of medicine in the United States, from neurosurgery to primary care. But we incorporate a difference in philosophy in that we approach each person from a whole-person perspective. Osteopathic medicine addresses healthcare for the mind, body, and spirit of every patient, so it makes perfect sense for us to elevate mental health care education as part of our curriculum.”
It’s not just its commitment to elevating mental health care education that will set the college apart. Specifically, it’s how it will accomplish it. At the heart of IllinoisCOM’s curriculum, for example, will be a longitudinal Mind and Medicine course that spans all four years of medical school.
“Our Mind and Medicine course is a multifactorial, interdisciplinary course that will utilize a bunch of different teaching methodologies,” explains Dr. Lucas, who says the course at various points will incorporate asynchronous learning, small-group instruction, and even laboratory work. “It will be taught not just by physicians, but also by psychologists. And it will address a ton of different topics … that profoundly impact a person’s health, including things like stress and socioeconomics.”
Plans for the college include a pharmacogenomics laboratory dedicated to exploring precision-medicine interventions for mental health care patients, for whom the efficacy of antidepressants and other drugs may depend on genetic factors. Mental health care also will figure prominently in cocurricular service projects, and in new-student orientations. As part of their initial weeklong orientation, for example, new students entering the IllinoisCOM will be required to complete QPR—question, persuade, and refer—training for suicide prevention. And within their first month of medical school, students likewise will receive nine hours of mental-health first-aid training.
“We won’t be able to drive positive mental health care outcomes for patients until we train our providers to talk openly about mental health as a critical component of wellness,” Dr. Kinde says. “By giving our students from day one a safe learning environment in which to talk about some really uncomfortable things, we’re normalizing the behavioral health skills and behaviors they’ll need so they can eventually transfer them into clinical practice.”
Cutting-Edge Coursework
Technology will play a pivotal role in mental health care education at the IllinoisCOM, promises Associate Dean for Clinical Simulation James Colquitt, Ph.D.
“My specialty in the medical education field is experiential learning,” Dr. Colquitt says. “Rather than having students’ first exposure be with actual patients experiencing mental health crises, we create simulated experiences. These use human actors, manikins, and artificial intelligence- and virtual reality-based systems. Through these realistic scenarios, students develop the confidence and competence needed to address mental health problems in the real world.”
At the heart of AI- and VR-based simulations will be virtual patients presenting with behavioral health challenges that students will have to identify and triage while also developing a professional and trustworthy bedside manner, according to Dr. Colquitt, who says technology will figure most prominently during the preclinical phase of students’ medical education.
“Students’ first two years will focus on early clinical and simulated experiences to prepare them for their third year, when they’ll enter hospital rotations like any typical medical student,” Dr. Colquitt continues. “We believe these prior simulated experiences will better prepare them to handle the complex mental and psychological circumstances they’ll encounter with patients, giving them an advantage over traditionally trained medical students.”
Mindful Medical Students
Providers’ mental health is just as important as patients’ mental health, observes Dr. Kinde, who notes that physicians die by suicide at more than twice the rate of the general population. “Providers are leaving the profession, physician burnout is at an all-time high, and doctor resilience is decreasing,” she says.
To address this, the IllinoisCOM will divide students into learning communities, small groups of 10 or 12 peers with whom students can form social circles and study groups. Says Dr. Kinde, “We’ll also be integrating things like mindfulness, yoga, and reflective practices; hiring full-time mental health professionals who will have fully schedulable office hours for students’ use; and training our faculty and staff in the same practices that we’ll be teaching our students. Our faculty and staff will be our students’ primary mentors, so we want them to model the healthy behaviors that we want our students to reflect.”
In that way, mental health will be as much a part of the college’s culture as it is a part of its curriculum.
“The incidence of mental health issues within the med student population is significant and growing. So, we need to be able to teach students not only how to take care of their patients, but also how to take care of themselves,” Dr. Lucas says. “If we can do that, our students hopefully will become resilient physicians who have long and productive careers caring for the patients and communities who need them most.”
A Foundation for Success
While medical schools across the country are paying more attention to the mental health of students and patients, the IllinoisCOM will stand apart by being built on a foundation of a national university that’s been at the forefront of mental health for more than 45 years.
“We are the fourth college of The Chicago School,” Dr. Lucas says. “Our college is going to be in the same building as other disciplines taught at The Chicago School, so there will be incredible cross-pollination between our med students and psychology students, which hopefully will lead to expanded conversations and foundational respect for what each other does and the roles that both can play in the holistic healthcare picture.”
“We’re all really excited to tap into the phenomenal network of allied mental health professional trainees that exists at The Chicago School,” Dr. Kinde adds. “Integrating those trainees with our own trainees so they can learn from each other will help us demonstrate what integrated healthcare looks like so they can practice it long before they’re actually out in clinical practice.”
In addition, IllinoisCOM will be able to tap into the national community partnerships that The Chicago School has developed over nearly five decades. This will offer students the opportunity for clinical rotations near all of The Chicago School’s campus locations across the country.
When IllinoisCOM students do eventually arrive in clinical practice, their mental health training will contribute to an entirely new and better patient experience, predicts Associate Dean for Research and Clinical Simulation James Colquitt, Ph.D. “What if our model at IllinoisCOM becomes a national standard?” he asks. “I believe we’d transform healthcare into something more personal, where empathy and understanding become fundamental to patient care rather than afterthoughts.”
He speaks from personal experience. “I met with my own physician a few months ago—an osteopathic doctor who exemplified what I believe our graduates will practice,” Dr. Colquitt continues. “Our conversation wasn’t centered on medications or surgical interventions. Instead, we discussed behavioral changes I could make to improve my long-term health, and how my healthcare team—physician, dentist, and therapist—could collaborate to address my wellbeing comprehensively. This integrated, person-centered approach represents the healthcare system we’re striving to build through our work at IllinoisCOM.”